Liver Lobe Torsion in Rabbits
Liver lobe torsion is a problem that can occur in many different kinds of animals, including dogs, cats, rabbits, pigs, horses, rats, and humans. The liver is comprised of many different lobes. Liver lobe torsion occurs when a lobe twists on itself, cutting off circulation to that part of the liver. This results in the release of liver enzymes as those cells die off. Eventually this can lead to shock and death. In rabbits, liver lobe torsion occurs infrequently, though it seems to be diagnosed more frequently in the Greater Boston area.
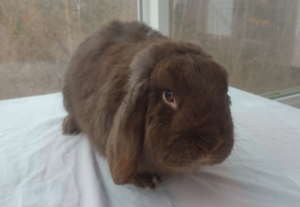
We don’t know why some rabbits experience this particular problem, or why we see it more commonly in New England. It’s possible that some rabbits are born without ligaments that support the liver, or that these ligaments could be stretched by trauma or disease. We do know that it seems to occur more commonly in mini-lop rabbits. Unfortunately, we haven’t been able to track the lineages of these rabbits to see if there’s a common ancestor. It’s also possible that there are more reported cases of liver lobe torsion in New England rabbits because we have the experts in this disorder practice at our referral institutions, and they have raised awareness of the disease in local veterinarians and veterinary students.
Liver lobe torsion can present with non-specific signs. Usually rabbits are brought to the vet for loss of appetite, lethargy, and decreased stool production of one day duration. These are the same reasons that many rabbits are brought to the vet and diagnosed with GI stasis. There are a myriad of problems that can result in GI stasis, including dental disease, poor diet, anesthesia, stress, pain, infection, and lead toxicity. In a perfect world, every rabbit that comes into the vet’s office with GI stasis would have bloodwork and x-rays performed. This doesn’t always happen, mostly because of financial concerns. So how do we know when to be more aggressive about pursuing these diagnostics? One of the key factors is abdominal pain, especially in the front part of the abdomen. Another is breed disposition – a mini-lop would raise the index of suspicion since they are overrepresented in the literature on liver lobe torsion in rabbits. Usually there is a range of severity of clinical signs on presentation, and clearly a rabbit that looks worse would warrant more aggressive intervention.
Liver lobe torsion can be diagnosed using a combination of bloodwork and imaging. On bloodwork, many rabbits with liver lobe torsion are anemic. All of them have moderately to severely elevated liver enzymes. Some have elevated kidney values as well, which could be attributed to dehydration. Radiographs may provide some clues, but findings can be non-specific. An abdominal ultrasound is the diagnostic modality of choice. An ultrasound can show enlargement of a liver lobe, rounded liver lobe margins, and a lack of blood flow to a particular lobe.
Once a diagnosis of liver lobe torsion is made, the treatment of choice is surgical removal of the affected liver lobe. Rabbits that are taken to surgery early do quite well. These rabbits are generally treated with fluid therapy, pain management, antibiotics, prokinetics to help with gut motility, and nutritional support. Some rabbits are not taken to surgery, either because of a delayed diagnosis or because of financial constraints. There are rabbits who are treated with medical management alone, but it is a long, labor intensive process to get them back to health. Many of these rabbits have a recurrence of GI stasis issues in the future, and some of them do not survive.
Liver lobe torsion is a diagnosis that should be considered in rabbits (especially mini-lops!) with GI stasis, abdominal pain, anemia, and elevated liver enzymes. Once a diagnosis is confirmed with ultrasound, surgery can have a successful outcome. While this disorder is relatively rare, we’re lucky to have experts in the field as local resources.
— Jacqueline Warner, DVM
